Should the Baby and the Yolk Sac Be the Same Size at 6 Weeks
Abstruse
Our objective was to prospectively validate the use of gestational sac (GS), yolk sac (YS) diameter, crown-rump length (CRL), and embryonal centre rate (60 minutes) dimensions to identify early pregnancy loss. This was a prospective cohort report of first trimester pregnancies. GS and YS bore, CRL, and Hour measurements were serially obtained in singleton and twin pregnancies from 6 through ten weeks' gestation. Non-parametric tests and logistic regression models were used for comparisons of distributions and testing of associations. A total of 252 patients were included, of which 199 were singleton pregnancies, 51 were twins, and 2 were triplets (304 full fetuses). 50-ii patients had 61 losses. We built nomograms with the changes of the parameters evaluated in ongoing, likewise as in pregnancy loss. In the pregnancies which failed, all the parameters showed meaning changes, with different temporal onsets: GS and YS were the first to become abnormal, deviating from normality as early as half-dozen weeks' gestation (OR 0.01, 95% CI 0.0–0.09, and OR three.36, 95% CI 1.53–vii.34, respectively), followed by changes in 60 minutes, and CRL, which became evident at vii and 8 weeks (OR 0.96, 95% CI 0.92–1.0, and OR 0.59, 95% CI 0.48–0.73, respectively). Our observations showed that, subsequently 5 complete weeks' gestation, a small GS and a big YS reliably predicted pregnancy loss. The YS reliably identified the occurrence of a miscarriage at least seven days prior its occurrence. CRL and Hr became abnormal at a later time in pregnancy and closer to the outcome. These findings take important implications for patient counseling and care planning, equally well equally a potential bearing on cost effectiveness within early pregnancy care.
Introduction
Early pregnancy loss - also known every bit pregnancy loss, fetal demise, miscarriage, or spontaneous abortion - is divers as a "nonviable, intrauterine pregnancy with either an empty gestational sac or a gestational sac containing an embryo or fetus without fetal heart activity prior to 12 weeks and 6 days of gestation"1. It is the nearly mutual complication of early pregnancy, affecting about 30% of pregnancies following assisted reproduction and 10% of spontaneously conceived pregnancies2,3,4. The difference is explained past a later diagnosis of spontaneous pregnancy versus assisted reproduction pregnancy, and an early loss is hands overlooked. In fact, vaginal bleeding - a common sign of early on pregnancy loss - tin be confused with delayed menses and the loss remains unrecognized. The about mutual cause of a beginning trimester pregnancy loss is embryonal genetic abnormalities, which occurs in more than 50% of the cases, with aneuploidy being the most frequent abnormality5,6.
Multiple serologic and ultrasound markers have been investigated to place pregnancies destined to be lost7,eight. Even so, serologic markers are unspecific and can aid but after a pregnancy loss has already been diagnosed. Transvaginal ultrasound (TVUS) provides loftier-resolution images, low inter-observer variability with high reliability, and is typically used to make diagnosis of intrauterine pregnancy and to follow up with its development9. Gestational sac (GS), yolk sac (YS), crown-rump length (CRL), and heart rate (HR) are the parameters measured to evaluate early on pregnancy. Deviations in the ultrasound parameters have been alternatively investigated to predict first trimester pregnancy loss. The amniotic sac, which becomes visible at the offset of the 7th calendar week of gestation, is usually non contemplated in the prediction models, nevertheless it assists in dating a pregnancy correctly.
Logistic models have been used to assess predictability of pregnancy loss using ultrasound parameters as dependable variables. One model including 566 gravidas, seven.9% of whom had an early pregnancy, identified HR and CRL as the most significant parameters to predict a pregnancy loss, together with maternal age and vaginal bleedingviii. Another i evaluated pregnancies accomplished by in vitro fertilization and plant that multiple variables including maternal historic period, elapsing of infertility, GS diameter, CRL, HR, and YS, predicted an early on pregnancy loss better than each individual parameters10. Yet, the model did not include an exact gestational age and included variables, such equally maternal age, which lonely is a well-established chance factor for commencement trimester pregnancy losseleven. Another model reported that a CRL, GS, and HR, below the 5th percentile, and a YS diameter above the 95th percentile would predict early pregnancy loss (odds ratio ane.04). Still, a normal YS would not decrease the risk of pregnancy loss when the other parameters were aberrant12. A systematic review evaluated sensitivities and specificities of the ultrasound parameters and institute that HR ≤ 110 beats per minute (BPM) was the most reliable model to predict a subsequent pregnancy loss, with a sensitivity of 68.4%, a specificity of 97.eight%, a positive likelihood ratio of 31.7 (95% conviction interval 12.8–78.8), and a negative likelihood ratio of 0.32 (95% conviction interval 0.sixteen–0.65). In pregnancies with vaginal haemorrhage, in addition to an HR ≤ 110 BPM, prediction of an early loss was higher13. All the discussed early on pregnancy ultrasound markers have been alternatively institute to predict first trimester loss, nevertheless they take never been evaluated longitudinally, and only 1 ultrasound per patient was included in the analysesten,13,14,15.
The yolk sac has been individually studied equally a marker of pregnancy loss. Being identified at approximately five weeks of gestation and gradually increasing in size in a linear fashion until 10 weeks of gestation, the YS is the first identifiable structure via transvaginal ultrasonography inside the GS. In particular, a YS larger than six.0 mm at any gestational historic period was associated with early loss, while an aberrant shape would non carry an ominous prognosis15,16. Our grouping established a nomogram of YS growth from its offset advent until ten weeks of gestation and constitute that deviations from the typical growth pattern were associated with a pregnancy loss17.
Previous studies were cross sectional and provided estimates for pregnancy loss that were based on a combination of ultrasound, besides as serologic and demographic markers. The aim of this written report was to estimate a hazard of offset trimester pregnancy loss based solely on ultrasound findings. Thus, we longitudinally evaluated the GS, YS, CRL, and 60 minutes changes in singleton and multiple pregnancies with definite conception dates in society to build nomograms of their changes up to 10 weeks of gestation. In improver, we wanted to place which parameters were the offset and virtually reliable to predict a pregnancy loss in singleton and multiple pregnancies. Our hypothesis was that unlike markers would sequentially become abnormal at different embryonal stages, when a pregnancy is destined to exist lost.
Materials and Methods
This was a prospective cohort study. The carry of this written report was approved by the Academy of Tennessee Wellness Scientific discipline Center Man Investigation Committee and the study is currently registered at ClinicalTrials.gov (NCT02429336). All methods were performed in accordance with the relevant guidelines and regulations. All patients gave informed, written consent to participate in the written report. The patients in our report were all evaluated and treated for infertility and had known conception dates. The mode of conception included spontaneous, later on superovulation with clomiphene citrate or letrozole with, or without, intrauterine insemination (IUI), and in vitro fertilization (IVF) after superovulation with gonadotropins. The GS and YS diameter, CRL, and HR measurements were obtained with 2-D transvaginal ultrasound in singleton, and multiple pregnancies followed from 6 through 11 weeks' gestation. For the scans we used ii ultrasound machines: Philips XD11 with a 7.5 MHz transvaginal probe and a Samsung UGEO WS80A 3-D with a vii.v MHz transvaginal probe. All measurements were obtained on a magnified, frozen department (sagittal and/or transverse) of the parameter to be evaluated. Measurements of the GS were obtained in three dimensions (length, height, width), the YS bore was measured from one inner rim to the contrary inner rim. If non spherical, the three dimensions were measured and averaged. The CRL was measured once and the FHR was measured once with One thousand mode. Both parameters' measurements were repeated in dissimilar sections if the first measurement did non meet the expected value for gestational age. The ultrasound motorcar provides the expected gestational age for each variable measured based on standardized algorithms, except for YS. For YS, we used the previously established nomogram of YS growth from v until 10 weeks of gestation17. Effigy ane shows the correct cursor position for the measurement of the parameters under investigation. The GS largest diameter was measured in the three orthogonal planes and averaged (Fig. 1A). The YS largest bore was measured placing the calipers at the inner rim of the organ. CRL was measured placing the calipers in the nearly cephalad and virtually caudal extremities of the embryo's longitudinal image. HR was automatically calculated by the car, averaging the distance betwixt one, or two, systolic spikes.
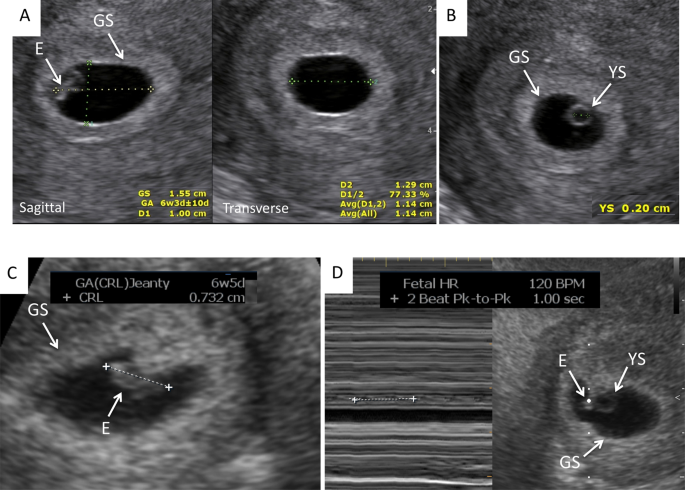
Right cursor position for the measurement of the parameters under investigation: (A) Gestational sac (GS); (B). Yolk sac (YS); (C). Crown-rump length (CRL); (D). Center Rate (60 minutes). Eastward = Embryo.
All the clinic patients with a positive pregnancy test were invited to come to the clinic for an initial transvaginal ultrasound at 5–6 weeks of gestation, depending of the patient'southward history. All patients presenting between January 2014 and December 2017 were included in the report. Most patients had weekly ultrasounds from 5 to eleven weeks of gestation, for an average of four scans per patient. To maintain consistency, a single examiner performed all of the sonographic exams of this study. If at the initial browse the embryo had no cardiac action, all parameters were measured to confirm the gestational age and a second scan was performed one week later on to confirm the outcome. If no gestational sac was present, and an ectopic pregnancy was excluded, or the mean gestational sac bore measured more than 20 mm without a visible YS or embryonal pole, these were classified as a nonviable pregnancy and were excluded from the analyses. In this cohort, there were no pregnancies that ended in elective termination.
Recurrent pregnancy loss was defined as two or more than first trimester pregnancy losses18. All pregnant women were discharged from the Reproductive Medicine clinic between 10 and 11 weeks of gestation. Pregnancy effect was determined through the evaluation of hospital medical records.
Statistical analysis
Variables, even if continuous, were expressed as Median and quartiles (Q1, Q3) because the Median is not skewed so much by a small-scale proportion of extremely large or small values and information technology is more than representative of a typical value. All analyses were performed using SAS/STAT V14.1 (Cary, N Carolina, USA). Mann-Whitney U test and Pearson correlations were used for comparisons betwixt the ongoing pregnancy and pregnancy loss groups (Tabular array 1). The GS and YS diameters, CRL and FHR were plotted relatively to gestational historic period. Descriptive statistics including medians and quartiles for GS, YS, CRL and HR for each gestational week were calculated by pregnancy loss condition. If a patient had a loss before and a continuing pregnancy after, she was allocated to the group which identified the outcome at the time of her pregnancy. If the patient had twins, or triplets, with 1 or ii losses within the same pregnancy (=vanishing twin), to balance the results she was allocated to both groups. We applied Wilcoxon two-sample tests past gestational calendar week for univariate comparison of distributions/medians for GS, YS, CRL, and Hr, between the pregnancies that were lost and those that were not. For YS, we also performed a median carve up analysis using Wilcoxon 2-sample tests past gestational calendar week both to a higher place and below the YS median, to compare the YS medians by pregnancy loss condition. We calculated the gestational age in weeks, rather than in days, considering it is the standard method to mensurate the gestational age in clinical practice. We extended the univariate analysis into multivariate logistic regression models in gild to retain multiple significant predictors of pregnancy loss by gestational week. Non-significant variables were omitted from the model unless contributing to the overall fit of the model. We estimated optimal sensitivity and specificity of each model along with surface area nether the receiver operating feature curve (AUC). All associations were considered significant at blastoff level 0.05.
Results
Of the 252 pregnancies included in this study, 199 (78.9%) were singleton pregnancies, 51 (20.2%) were twins (3 of which were monochorionic and 48 dichorionic), and two (0.008%) were triplets (monochorionic twins plus a singleton; both pregnancies spontaneously reduced to singleton at 7 weeks of gestation), for a total of 304 embryos longitudinally studied (i of the twin pregnancies had an empty GS, which was excluded from the calculations). Thirty-vi of 252 pregnancies (14.3%) had a commencement ultrasound between 4–five weeks of gestation because of history of ectopic pregnancy, recurrent pregnancy loss, pelvic pain, or vaginal bleeding. For 21 patients, no delivery information was bachelor, nonetheless they were lost to follow-upwards after their 3rd-trimester ultrasound and were included in the analyses in the group of patients who had a standing pregnancy.
60-one of 304 (xx%) embryos, in 52 pregnancies, were lost: 20/61 (32.8%) in twin, or triplet, pregnancies and 41/61 (67.ii%) in singleton pregnancies. The remaining 243 embryos progressed beyond the first trimester. 30-three of 61 embryos (54.one%) were already lost at the time of the initial ultrasound, of which xix (31.ane%) at iv–5 weeks and 14 (22.9%) at half dozen weeks of gestation. Of the pregnancies that were lost, only five had vaginal haemorrhage as the initial sign of pregnancy failure, all in singleton pregnancies. Neither of the twin pregnancies with a vanishing or demised twin underwent genetic assay. Of the 61 pregnancy losses, 18 singleton and i twin pregnancies underwent microarray assay for genetic abnormality: results were inconclusive in ii instances, and unknown in ane. Twelve of 17 (70.6%) showed chromosomal abnormalities: 4 were trisomy 21, 2 were trisomy 16, ii were trisomy 22, 2 were triploid, and 2 were complex genetic abnormalities. All embryos had a YS diameter larger than the median in continuing pregnancies pregnancies. Five of 17 (29.four%) were normal karyotypes and all embryos had smaller or similar YS diameter compared to the median in continuing pregnancies.
Tabular array 1 reports the demographics and the clinical characteristics of patients that had a first trimester pregnancy loss (Northward = 52, 61 lost embryos) and those who continued the pregnancy across the commencement trimester (Northward = 209, 243 fetuses). Variable measurements in the standing pregnancy group conformed to the expected value by gestational age calculated by the ultrasound auto and were considered the normal cutting-offs at each gestational age. Patients with twin/triplet pregnancies who lost ane, or 2, embryos, but continued the pregnancy with the remaining fetus/es (13/51 twins and 2/2 triplets) were allocated to both groups. In this way, maternal characteristics would take the aforementioned statistical weight in the two groups. At that place was no difference in age, BMI, gravidity, parity, mode of conception, and clinical history (all not significant to <0.05). Spontaneous conception was the most mutual fashion of conception in the pregnancy loss group, while IVF was the most mutual in the continuing pregnancy group; polycystic ovary syndrome was the about common preexisting clinical condition in both groups, followed by uterine subseptations. Seventy-one patients had had one, or ii, pregnancy losses prior to the index pregnancy. 20-six patients had a diagnosis of recurrent pregnancy loss (6 in the pregnancy loss, and 20 in the standing pregnancy group). Two twin pregnancies were delivered at 26 weeks of gestation: one for preterm delivery and the other for severe preeclampsia in a 44 year-old woman who had conceived through egg donation. 1 singleton pregnancy was included in the continuing pregnancy grouping fifty-fifty though it was complicated by fetal demise at 24 weeks from a tight nuchal cord. The fetus had a normal male karyotype, 46, XY. Fifty-eight additional fetuses were delivered between 32 and 36 6/7 weeks of gestation, mostly from preterm delivery of twin pregnancy (45 fetuses in twin pregnancies, and 13 fetuses in singleton pregnancies), and the remaining 180 fetuses were delivered at term (≥37 weeks of gestation). None of the neonates had genetic abnormalities. All the investigated parameters became significantly different in pregnancies destined to be lost, but with a dissimilar chronology. Aside from the GS dimensions in monochorionic twins, there was no difference in dimension of whatever other parameters in singleton versus multiple pregnancies.
Figure 2 shows the median GS, YS, CRL, and 60 minutes measurements at the gestational ages under investigation in the two groups, pregnancy loss and standing pregnancy. Variable measurements in the continuing pregnancy group conformed to the expected gestational historic period by the ultrasound machine and were considered the normal cut-offs at each gestational age. The GS bore grew 6.65 mm per week (R2 = 0.9979) in pregnancies that continued across the outset trimester and it was smaller in pregnancies destined to exist lost, nonetheless the difference was not significant until 8 weeks of pregnancy, when the median diameter of the gestational sac was xv mm (IQR 12, 21 mm) in pregnancy losses and 31 mm (28, 35 mm) in continuing pregnancies (p < 0.001, Fig. 2A, Table 2). The YS grew 0.38 mm per week (Rtwo = 0.9983) in pregnancies that connected beyond the first trimester. In pregnancies destined to be lost, the YS was either smaller, or larger, than in continuing pregnancies starting at 5 weeks of gestation, and maintained the trend until the pregnancy loss was diagnosed (Fig. 2B, Table two). The CRL grew 7.54 mm (R2 = 0.9903) per week and was significantly larger in the continuing pregnancy than in the pregnancy loss group from 6 through 10 weeks (Fig. 2C, Tabular array 2). HR increased from 5 weeks of gestation and became significantly unlike in the two groups between vii and viii weeks of gestation, when it increased by 13 BPM in the standing pregnancy, versus increasing three BPM in the pregnancy loss group. HR still fit a linear relationship with gestational age, increasing by 13.76 BPM per week, even though with a lower R2 of 0.8637.
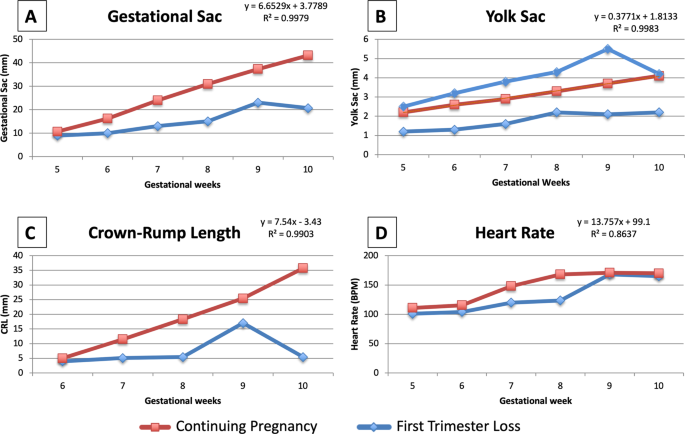
Median measurements of the parameters under investigation in the two groups, pregnancy loss and continuing pregnancy, plotted confronting the gestational age: (A). Gestational sac (GS); (B). Yolk sac (YS); (C). Crown-rump length (CRL); (D). Heart Rate (HR).
Univariate comparisons are reported in Tabular array 2. In early gestational weeks (weeks seven and 8), a larger median YS was associated with an increased risk of pregnancy loss, whereas in week ten, a smaller median YS was associated with an increased adventure of pregnancy loss. Starting at half dozen weeks of gestation up to 10 consummate weeks, smaller GS and CRL were associated with a subsequent pregnancy loss (p < 0.01 for all). A slower HR was predictive of a subsequent pregnancy loss at seven through viii weeks of pregnancy (p < 0.05 for both), notwithstanding, this did non concord true for a slower HR occurred prior to seven weeks or after 8 weeks.
This assay farther confirmed our findings when we subdivided the pregnancy loss group into those beneath and above the expected YS median per gestational age. In fact, a smaller YS bore was associated with pregnancy loss at week vi (trend), and 8–10 of gestation (p < 0.05 for all), and a larger YS diameter was associated with pregnancy loss from week half dozen–9 of gestation (p < 0.05 for all; Tabular array 3). Figure 2B reports the YS diameter of pregnancy losses at different gestational ages compared to continuing pregnancies. Figure 3 shows ultrasound and hysteroscopic images of an enlarged YS in a 69, XXY pregnancy. Using the significant univariate models and later excluding 19 pregnancy losses diagnosed at the time of the initial ultrasound, 43% of the losses (18/42) could be predicted at least one week before they occurred. In particular, a smaller GS, a shorter CRL, and a larger YS, could predict 43% of the pregnancy losses 1 week in advance in 9 cases, 2 weeks in accelerate in seven cases, iii weeks in advance in 1 example, and 5 weeks in advance in one example. A slow embryonal Hr was not handsomely anticipatory of a loss.

(A) Ultrasound and hysteroscopic images of the yolk sac in a partial mole pregnancy (Karyotype: 69, XXY at microarray analysis). (A) Ultrasound picture showing an enlarged yolk sac at half-dozen weeks and one solar day of gestation; (B). Ultrasound picture showing an enlarged yolk sac at 8 weeks and 2 days of gestation; (C). Hysteroscopic view of the yolk sac at the fourth dimension of pregnancy evacuation at 8 weeks and 2 days of gestation, later on embryonal demise. (D) A portion of the yolk sac tin be noted just outside of the amniotic sac, with the embryo within it, in the groundwork. GS = gestational sac; YS = yolk sac.
Results of the logistic regression models for the multivariate analysis are displayed in Tabular array four. These regressions were performed by gestational week, with pregnancy loss every bit the outcome variable. Sensitivity and specificity were estimated from the models, AUC is presented as a measure of model fit. These adjusted models largely confirm the univariate findings. A larger YS was associated with a 3–6 times increased run a risk of pregnancy loss from v through viii weeks. At 10 weeks of gestation, instead, a larger YS was associated with a decreased gamble of pregnancy loss. This is reflected in the fact that just one pregnancy loss after ten weeks of gestation had an enlarged YS. In fact, all the losses at that gestational age showed a YS smaller than the median for pregnancies continuing beyond the starting time trimester. A larger GS was associated with a decreased chance of losing the pregnancy, suggesting that a smaller GS, instead, is indicative of pregnancy loss. The direction of this clan was consistent over the time frame under investigation, reaching significance at, 6, 7, and ix weeks. Similarly, a larger CRL measurement was associated with a decreased adventure of pregnancy loss, over again indicating that a smaller CRL at 8 and nine weeks of gestation predicts a pregnancy loss. The models performed with reasonable predictive accurateness and goodness of fit. Sensitivity ranged from 60–86% and specificity from 78–91%.
Word
In pregnancies destined to be lost, unlike ultrasound markers became abnormal at least one calendar week before the loss. Nosotros established that the GS, CRL, and YS are the first parameters to go abnormal, as early as 5 weeks of gestation, and that Hour becomes abnormal at a after time and only for a brief period prior to the loss. In improver, multiple markers predict the outcome with increased sensitivity and specificity compared to each individual marker.
The pregnancy loss rate of twenty% in our report was comparable to the one reported for IVFii, but college than the 1 reported for spontaneous pregnancies (about 10%)three,4. All the same, in our cohort about losses occurred inside 14 days of the missed catamenia, and in different circumstances where the conception date is not known, a pregnancy, and hence a pregnancy loss, would most often go unrecognized. The fact that spontaneous conception was the about mutual mode in the pregnancy loss grouping, while IVF was the most common in the continuing pregnancy group could be due to the dissimilar support of the luteal stage and early pregnancy stages, as IVF pregnancies are supported with gonadotropins prior to, and progesterone later, the solar day after oocyte retrieval (corresponding to the day of ovulation in spontaneous pregnancies), which change the endometrial characteristics compared with spontaneously conceived pregnancies. Polycystic ovary syndrome was the most common preexisting clinical status in both groups; it was treated in all patients with daily metformin, 500 mg to 2000 mg. These results might assist understanding the etiology of pregnancy loss in women with this condition, which in our report, seemed to be unrelated to the hyperinsulinemic condition, frequently reported equally the most probable cause of pregnancy loss19. However, studies powered to explore our incidental finding would be needed.
The YS appeared to be the strongest marker for the prediction of a pregnancy loss. Other studies have established YS as a reliable predictor of pregnancy result, nonetheless these studies are limited past their cantankerous-sectional evaluation with but i ultrasound per patient10,12,13,14,15,xvi. In our study we performed multiple ultrasounds to accurately correspond all gestational ages in each patient. Nosotros previously described a nomogram of YS evolution during the first 10 weeks of pregnancy with serial ultrasounds in pregnancies that continued beyond the kickoff trimester17. We confirmed a YS linear growth of approximately 0.iv mm per week in this larger patient sample. Our findings approve a large cantankerous sectional report with over 4,000 patientstwenty. After 5 complete weeks of gestation, the YS reliably detects pregnancies destined to exist lost, also confirmed by multivariate assay. In pregnancies destined to fail, the YS was either smaller or larger than in pregnancies continuing beyond the first trimester. While all pregnancies with a big YS were lost inside 10 weeks, some pregnancies with smaller YS were lost beyond 10 weeks of pregnancy. The etiology of a large YS is essentially unknown, however 18–66% of large YS diameters greater than 5–half dozen mm have been associated with abnormal karyotypes21,22. Our express genetic results seem to corroborate these previous findings.
CRL is difficult to measure out at 6 weeks of gestation, being discipline to the sonologist'south experience and the ultrasound car's capabilities. Several nomograms for CRL have been developed in dissimilar countries past cantankerous sectional studies. An international nomogram of CRL growth was recently developed for pregnancy dating, withal measurement started at ix weeks of gestation23. Betwixt 6 and 10 weeks of gestation, another cross exclusive study found a quadratic relationship between CRL and gestational age20. Our results, dating from 5 weeks of gestation, defined a linear fit of CRL growth, up to 10 weeks. CRL was a weak predictor of pregnancy loss between 6 and 8 consummate weeks of gestation, however it became a stronger predictor when combined with YS or GS abnormalities. In improver, the growth lag unremarkably preceded the event by less than one week, thus providing trivial fourth dimension for counseling.
Many HR nomograms have been developed, and one with the largest data was by Papaioannou20. In this cantankerous sectional study a cubic association between HR and gestational age was institute. Even so those pregnancies were followed through thirteen weeks of gestation, when a natural slowing in Hr is observed. We described a linear human relationship through 10 weeks of gestation with an excellent R2 value. Given the rather of import variation in BPM per 2d, a slower Hr is non a reliable tool to predict the occurrence of a pregnancy loss unless it is below 100 BPM at a gestational age greater than 6 weeks of gestation24. In our study, a 60 minutes slower than in continuing pregnancies was predictive of a subsequent pregnancy loss but between 7 and 8 weeks of gestation, merely non prior, or subsequently, this time. Even if highly specific of pregnancy loss when absent-minded, HR abnormalities presented very close to the event, thus providing little time for counseling.
A major strength of our study is the advantage of a single investigator performing all the ultrasounds, thus maintaining consistency in the measurements, with small inter-observer variability. Additionally, all subjects included in the study had precisely known gestational ages farther strengthening the accuracy of our results. Limitations of the report include the relatively modest sample size, along with a patient population treated for infertility, which may make our results not generalizable to spontaneous conceptions. Additionally, some pregnancies were already lost at the time of the first ultrasound at 5 or six weeks of gestation, and nosotros were not able calculate the interval betwixt the measured aberrant parameter and the loss. In fact, our model was suitable more often than not for pregnancies that had an ultrasound at vi weeks and were lost at eight–ix weeks of gestation, or later. We analyzed the data 'per calendar week' of gestation to reverberate the standard gestational age quantification, however, we may have lost sharpness of the results as compared to analyzing the data 'per day' of gestation.
In conclusion, we were able to establish a statistical model using only early on pregnancy ultrasound markers to predict a first trimester loss. GS and YS were the earliest parameters that could reliably exist used as prognostic factors for pregnancy loss, every bit they became abnormal as early every bit vi weeks of gestation with loftier sensitivity and specificity. Of all the evaluated parameters, the YS was the strongest unmarried predictor. These findings are clinically useful for patient counseling and determining the need for closer monitoring. In fact, if these parameters are normal at vi weeks, the pregnancy will probable go on beyond the first trimester. Although needing prospective validation, our results support changing the electric current standard of care of performing the first obstetric ultrasound at 9 weeks of gestation to half-dozen weeks of gestation. If the YS and the GS are normal, a provider can offer reassurance concerning the decreased likelihood of a pregnancy loss.
Alter history
-
28 October 2021
A Correction to this paper has been published: https://doi.org/ten.1038/s41598-021-01235-0
References
-
American Higher of Obstetricians and Gynecologists. Early pregnancy loss. Do Bulletin No. 150. Obstet & Gynecol 2015; 125, 1258–1267. Retrieved February 15, 2018, from, http://www.acog.org/Resource-And-Publications/Do-Bulletins/Committee-on-Practise-Bulletins-Gynecology/Early-Pregnancy-Loss.
-
Orvieto, R. et al. Outcome of pregnancies derived from assisted reproductive technologies: IVF versus ICSI. J Assist Reprod Genet 17, 385–387 (2000).
-
Wang, X. et al. Conception, early pregnancy loss, and fourth dimension to clinical pregnancy: a population-based prospective report. Fertil Steril 79, 577–84 (2003).
-
Zinaman, One thousand. J., Clegg, E. D., Dark-brown, C. C., O'Connor, J. & Selevan, S. G. Estimates of human fertility and pregnancy loss. Fertil Steril 65, 503–9 (1996).
-
Lathi, R. B. & Milki, A. A. Tissue sampling technique affects accuracy of karyotype from missed abortions. J Assist Reprod Genet 19, 536–538 (2002).
-
Zhang, H. G. et al. Assay of fetal chromosomal karyotype and etiology in 252 cases of early on spontaneous abortion. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 28, 575–578 (2011).
-
Lek, Southward. Grand. et al. Validation of serum progesterone <35 nmol/Fifty as a predictor of miscarriage amid women with threatened miscarriage. BMC Pregnancy Childbirth 17, 78–84 (2017).
-
Tarasconi, B. et al. Serum antimüllerian hormone levels are independently related to miscarriage rates later on in vitro fertilization-embryo transfer. Fertil Steril 108, 518–524 (2017).
-
Pexsters, A. et al. Clinical implications of intra- and interobserver reproducibility of transvaginal sonographic measurement of gestational sac and crown-rump length at half dozen–ix weeks' gestation. Ultrasound Obstet Gynecol 38, 510–5 (2011).
-
Yi, Y. et al. A logistic model to predict early pregnancy loss following in vitro fertilization based on 2601 infertility patients. Reprod Biol Endocrinol 14, 15 (2016).
-
Khalil, A., Syngelaki, A., Maiz, N., Zinevich, Y. & Nicolaides, One thousand. H. Maternal age and agin pregnancy outcome: a accomplice study. Ultrasound Obstet Gynecol 42, 634–43 (2013).
-
Datta, Grand. R. & Raut, A. Efficacy of start-trimester ultrasound parameters for prediction of early spontaneous ballgame. Int J Gynaecol Obstet 138, 325–330 (2017).
-
Pillai, R. N., Konje, J. C., Richardson, Chiliad., Tincello, D. G. & Potdar, N. Prediction of miscarriage in women with feasible intrauterine pregnancy—A systematic review and diagnostic accuracy meta-assay. Eur J Obstet Gynecol Reprod Biol 220, 122–131 (2018).
-
Stamatopoulos, N. et al. Prediction of subsequent pregnancy loss adventure in women who present with a feasible pregnancy at the first early pregnancy scan. Aust North Z J Obstet Gynaecol 55, 464–72 (2015).
-
Tan, Due south. et al. Aberrant sonographic appearances of the yolk sac: which tin be associated with adverse perinatal consequence? Med Ultrason 16, fifteen–20 (2014).
-
Ashoush, Southward., Abuelghar, West., Tamara, T. & Aljobboury D. Relation between types of yolk sac abnormalities and early embryonic morphology in first-trimester missed pregnancy loss. J Obstet Gynaecol Res., 42(one), 21–8, https://doi.org/10.1111/jog.12837 (2016 January).
-
Detti, L. et al. Pilot study establishing a nomogram of yolk sac growth during the offset trimester of pregnancy. In Press, Journal of Obstetrics and Gynecology Research (2019).
-
Definitions of infertility and recurrent pregnancy loss: a commission opinion. Fertil Steril, 99, 63 (2013).
-
Goodman, North. F. et al. American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Androgen Excess and PCOS Lodge. American association of clinical endocrinologists, American college of endocrinology, and Androgen Excess and PCOS Society illness land clinical review: Guide to the best practices in the evaluation and treatment of polycystic ovary syndrome - Part 2. Endocr Pract 21, 1415–26 (2015).
-
Papaioannou, M. I., Syngelaki, A., Poon, L. C., Ross, J. A. & Nicolaides, 1000. H. Normal ranges of embryonic length, embryonic heart charge per unit, gestational sac bore and yolk sac diameter at half-dozen-10 weeks. Fetal Diagn Ther 28, 207–19 (2010).
-
Goldstein, S. R., Kerenyi, T., Scher, J. & Papp, C. Correlation betwixt karyotype and ultrasound findings in patients with failed early on pregnancy. Ultrasound Obstet Gynecol eight, 14–317 (1996).
-
Yoneda, S. et al. A Yolk Sac Larger Than v mm Suggests an Abnormal Fetal Karyotype, Whereas an Absent Embryo Indicates a Normal Fetal Karyotype. J Ultrasound Med 37, 1233–41 (2018).
-
Papageorghiou, A. T. et al. International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st). International standards for early fetal size and pregnancy dating based on ultrasound measurement of crown-rump length in the first trimester of pregnancy. Ultrasound Obstet Gynecol 44, 641–viii (2014).
-
Doubilet, P. M., Benson, C. B. & Chow, J. S. Long-term prognosis of pregnancies complicated past irksome embryonic heart rates in the early first trimester. J Ultrasound Med 18, 537–41 (1999).
Acknowledgements
This study was supported by an institutional grant from the Academy of Tennessee Health Science Middle, Memphis, TN (E07-3225-001).
Author information
Affiliations
Contributions
L.D. Research idea, Figures, Tables, Manuscript writing. L.F., Grand.E.C. and I.P.-A. Enquiry deport, Manuscript writing.. P.J.G. Statistical analysis, Tables, Manuscript writing. Z.B. Statistical analysis. R.A.R. Research conduct, Manuscript writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Boosted information
Publisher'due south note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Commodity was revised: The original version of this Article contained an mistake in the spelling of the writer Patricia J. Goedecke which was incorrectly given equally Patricia J. Goeske.
Rights and permissions
Open up Access This article is licensed under a Artistic Eatables Attribution 4.0 International License, which permits use, sharing, accommodation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original writer(s) and the source, provide a link to the Creative Eatables license, and indicate if changes were fabricated. The images or other third party fabric in this article are included in the article's Creative Commons license, unless indicated otherwise in a credit line to the material. If cloth is not included in the article's Creative Commons license and your intended use is not permitted past statutory regulation or exceeds the permitted employ, y'all will demand to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this commodity
Cite this article
Detti, 50., Francillon, L., Christiansen, M.E. et al. Early pregnancy ultrasound measurements and prediction of first trimester pregnancy loss: A logistic model. Sci Rep 10, 1545 (2020). https://doi.org/10.1038/s41598-020-58114-3
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1038/s41598-020-58114-3
Further reading
Comments
Past submitting a comment yous agree to abide by our Terms and Community Guidelines. If you observe something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Source: https://www.nature.com/articles/s41598-020-58114-3
0 Response to "Should the Baby and the Yolk Sac Be the Same Size at 6 Weeks"
Post a Comment